A dietary supplement too important to ignore.

Key questions answered in this article:
Why is CoQ10 so important?
Is supplementation a good idea for most people?
Has CoQ10 been shown to reduce mortality in randomized, placebo-controlled clinical trials?
The content below was originally paywalled.
One of the oft-repeated arguments against nutritional supplements is that they achieve nothing except more expensive urine.
I'm sure the people who say this believe, in their own minds, that they are being clever. Maybe even humorous. In reality they are confirming they know nothing of value about the topic and really should refrain from commenting any further until they do.
The question is not whether humans benefit from nutritional supplements, but "which humans need what supplements?"
Due to very wide variation in dietary intake, lifestyle habits, activity levels, psychosocial stresses, substance use and abuse, exposure to environmental toxins and genetic make-up, intake and bodily levels of the same nutrient can vary widely from person to person.
Dark-skinned people living in areas with low sunlight exposure are more likely to require supplemental vitamin D, as are elderly folks in temperate climates who spend little time outdoors.
Vitamin A is another often-overlooked nutrient. It has never been a 'trendy' supplement choice - in fact, even folks generally supportive of supplementation often warn against taking retinyl palmitate due to greatly overblown concerns about liver toxicity. Which is a pity, because only 46% of Americans meet the minimal RDA for vitamin A intake.
Another key micronutrient often lacking in modern diets is magnesium (Mg). Relatively few foods are rich in magnesium, and with the understandable popularity of filtered water (which renders water "soft" and low in minerals) it's little wonder only 43% of Americans meet the RDA for Mg. If you've got kidney issues or a heavy drinking habit, or take medications like diuretics or proton pump inhibitors, your chances of being Mg deficient are even higher.
People who eat little to no meat are far more likely to consume insufficient creatine, carnitine, carnosine, CoQ10, preformed vitamin A, vitamin B12 and long-chain n-3 fatty acids. While "eat more meat, duh!" might seem like an obvious response, bear in mind those who insist vitamin supplements are unnecessary are typically the same people who claim meat is bad and that soy/cereal fiber/refined vegetable oils are good for you. These people warn you away from nature's most nutrient-dense food, encourage you to replace it with foods high in anti-nutrients, while simultaneously claiming you don't need nutrient supplements.
Pure genius.
Whether or not you need to supplement a particular vitamin or mineral or trace element is an individual matter. In an ideal world, we'd undergo regular blood testing to see how we're travelling in terms of nutrient status. Of course, that's not the world we live in. Modern "blood work" is heavily geared towards finding "risk factors" that can then be used to push us onto pharmaceutical drugs.
This is because modern medicine is geared towards enriching its true owner: The pharmaceutical industry.
Given the prevailing inability to obtain individualized nutrient analyses, we’re left to embrace a scatter gun approach to supplementation.
This is why the standard recommendations for supplementation include a multivitamin/mineral product as a form of nutritional "insurance" to "cover your bases," along with recommendations to take extra supplements with a low risk of toxicity such as magnesium and vitamin D (during winter).
It's something of a hit-and-miss approach which reduces our odds of deficiency, but may still fall short on certain nutrients that we may have a high individual need for.
It may also over-deliver on other nutrients already sufficient in our diets. For example, many multivitamin/mineral supplements still contain iron. For reasons I've outlined here, unless you have a documented iron deficiency then taking supplemental iron is not a good idea. If you are already iron-replete, taking even more iron is likely to do more harm than good.
In light of all this, there is one supplement I consider largely non-negotiable for adults, and that's Coenzyme Q10, or CoQ10.
The reason for this is because CoQ10 deficiency is largely a matter of ageing, rather than diet.
Controlled clinical trials suggest correcting this deficiency might just save your life.
The Importance of CoQ10
To understand why supplementation is a good bet for most people, it's important to understand a few basic facts about CoQ10.
CoQ10 is an essential cofactor of enzymes involved in energy production within cells - hence the "coenzyme" designation. The conversion of energy from carbohydrates and fats to adenosine triphosphate (ATP), the form of energy used by cells, requires the presence of CoQ10.
CoQ10 concentrations are highest in mitochondria-rich tissues and organs with high energy needs such as the heart, liver and kidneys. While you sleep, these organs keep chugging away to keep you alive and healthy.
CoQ10 is also a fat-soluble antioxidant that protects cell membranes and lipoproteins from oxidative damage.
CoQ10, in short, is a critically important nutrient.
Which is why the age-related decline in CoQ10 levels should be of concern to anyone who cares about their health.
Although some CoQ10 (approximately 25% of our requirement) is obtained from the diet, most is manufactured within the body, particularly by the liver. A 1997 report estimated that the population of Denmark, for example, obtained only 3–5 mg of CoQ10 per day from their normal dietary sources. Synthesis of CoQ10 is a complex process requiring numerous amino acid, vitamin and trace element precursors and cofactors; a deficiency in any of these can adversely affect production of CoQ10.
As people age, the capacity of the body to produce CoQ10 decreases. CoQ10 levels can also be depleted by intense exercise, certain types of prescription drugs, and by illness.
In a landmark 1989 paper, Kalén et al from the Karolinska Institute in Sweden examined CoQ10 and lipid levels in autopsied individuals aged 1 day to 81 years of age. Excepting the pancreas and adrenal glands, their results indicated a peak in organ levels of CoQ10 at around age 20, followed by a steady decline with advancing age.
Below is a graph depicting the decline in liver, lung, kidney and heart CoQ10 concentrations observed by the Swedish researchers.
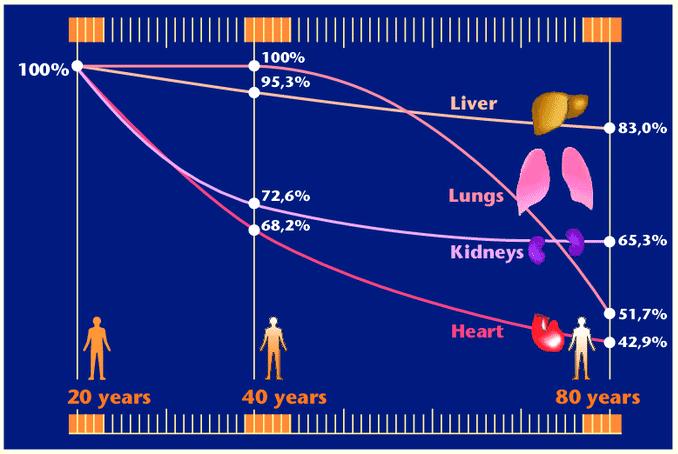
As you can see from the graph, especially large declines were observed in lung, kidney and heart concentrations of CoQ10. Obviously, we want to do everything in our power to keep these organs motoring along as efficiently as possible for as long as possible.
Low CoQ10 Levels and Risk of Illness
Compared to healthy subjects, low blood CoQ10 concentrations are seen in critically ill patients with or without sepsis.
Low blood CoQ10 concentrations have been reported as an independent predictor of in-hospital and post-hospitalization mortality and mortality in patients with chronic heart failure and acute cardiovascular disease.
Which begs the obvious question: Can CoQ10 supplements reduce mortality from these conditions?
Before we discuss whether or not supplementation helps, let’s talk about something you should scrupulously avoid if you wish to maintain optimal CoQ10 status.
Reason #3,675 Why Statin Drugs Suck
I’ve been warning against cholesterol-lowering statin drugs for over twenty years. These drugs were known to lower bodily levels of CoQ10 before they even hit the market. In 1989, Merck & Co., Inc. filed two patents for the use of CoQ10 with statins in order to prevent CoQ10 depletion and attendant side effects (see here and here). They never acted upon the patents, possibly because they didn't want to draw attention to the fact statins depleted levels of such an important enzyme. Anything that depletes your body of something so important as CoQ10 is not a good thing - it’s a toxin to be avoided at all costs.
Numerous studies have confirmed statin use causes significant declines in blood CoQ10 levels (for examples, see Berthold 2006, Mabuchi 2005, Chu 2006).
Statins are notorious for causing muscle pain and myalgia, and the CoQ10 depletion caused by these drugs is considered a major reason why.
Mixed results have been observed in the numerous studies where CoQ10 has been administered to statin users. That’s the problem: The patients were being given CoQ10 while still using statin drugs. That’s like trying to remove water from a sinking boat with a bucket while leaving the gaping hole unattended.
In 2005, Texas cardiologist and researcher Peter Langsjoen and colleagues published a report on fifty patients who had discontinued statins and commenced taking CoQ10.
All fifty patients had presented with one or more statin-related adverse effects as their chief complaint, so statin drug therapy was discontinued.
All patients were instructed to begin taking CoQ10 daily, at an average dose of 240 mg per day.
After an average follow-up of twenty-two months, the prevalence of fatigue dropped from 84% to 16%, myalgia from 64% to 6%, dyspnea from 58% to 12%, memory loss from 8% to 4% and peripheral neuropathy from 10% to 2%.
There were two deaths from lung cancer and one death from aortic stenosis but no strokes or myocardial infarctions. Measurements of heart function either improved or remained stable in the majority of patients. Langsjoen and his co-authors concluded: “... statin-related side effects, including statin cardiomyopathy, are far more common than previously published and are reversible with the combination of statin discontinuation and supplemental CoQ10. We saw no adverse consequences from statin discontinuation.”
I’ll reiterate: If you want to maintain optimal CoQ10 levels, give cholesterol-lowering drugs a wide berth.
How Has CoQ10 Performed in Clinical Trials?
This series looks at the effect of nutrient supplements on mortality. Studies in which healthy individuals are given a supplement or placebo to consume for decades on end, and followed for mortality outcomes, are pretty much non-existent.
Clinical trials tend to focus on individuals with a particular disease, those considered at higher risk of that disease, or elderly populations. In these groups, it’s a safe bet that morbidity and mortality will be higher during a given period compared to what would be observed in a healthy, low-risk population. This reduces the time-frame needed to detect differences in clinical endpoints between treatment and control groups.
CoQ10 has been most widely studied in RCTs for its ability to reduce morbidity and mortality from heart failure. Most of the trials have been very small, with less than 80 participants; very few featured more than 150 subjects. Meta-analysis of these trials suggests a benefit of coenzyme Q10 on all-cause mortality, with a relative risk reduction of 32%.
I’ll quickly discuss the larger trials below.
Morisco et al 1993
Italian researchers randomly assigned 641 patients with heart failure (New York Heart Association functional class III and IV) to receive either a placebo or CoQ10, in addition to their standard therapy. The male and female subjects ranged in age from 26-89 years (mean age 67).
In this double-blind trial, the CoQ10 dosage was 2 mg/kg per day. Given that the mean body weight was 69 kg, this equated to an average dose of 138 mg per day.
The type/brand of CoQ10 supplement was not reported, nor were changes in blood CoQ10 levels during the study.
At twelve months, 16 patients (5%) died in the CoQ10 group compared to 21 (6.5%) in the control group. The difference was not statistically significant.
There were, however, statistically significant differences in other outcomes.
The number of patients who required hospitalization for worsening heart failure was much smaller in the CoQ10 group than in the control group (23% versus 37%, respectively).
Similarly, episodes of pulmonary edema or cardiac asthma were greatly reduced in the CoQ10 group compared to the placebo group (6.3% versus 16%, and 30% versus 61%, respectively).
The Q-Symbio Trial
In a trial involving European, Asian, and Australian centers, 420 heart failure patients (NYHA class III or IV) were randomly assigned to 300 mg CoQ10 daily or placebo.
The CoQ10 supplement was a product called Bio-Quinone produced by Danish company Pharma Nord; each soft gelatine capsule contained 100 mg of CoQ as ubiquinone with 400 mg of soy bean oil.
In order to maintain elevated blood levels of CoQ10, one capsule was taken 3 times daily.
The study was partly funded by Pharma Nord and Kaneka, a Japanese manufacturer that mass produces the ubiquinone and ubiquinol forms of CoQ10 for supplement companies.
At week 16, serum CoQ10 levels remained unchanged in the control group but had risen from 1.14 mcg/ml to 3.01 mcg/ml in the treatment group. At 106 weeks, serum CoQ10 averaged 2.01 mcg/ml in the supplemented group.
At 106 weeks, the survival status of all patients was known, save for 4 patients in each group who were lost to follow-up. Sixty patients had died; 21 (10%) in the CoQ10 group, versus 39 (18%) in the placebo group.
As the figure below shows, there were far fewer heart failure deaths in the CoQ10 group. Sudden cardiac and stroke deaths were also lower in the CoQ10 group.
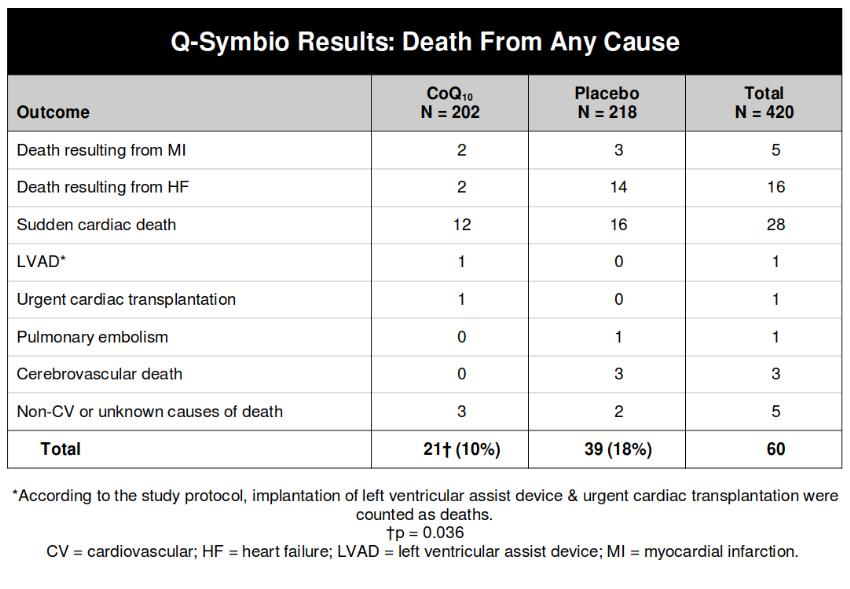
In addition, the need for hospitalization due to worsening heart failure was halved in the CoQ10 group.
The KISEL-10 Trial
Starting in 2003, Swedish researchers administered CoQ10 and selenium, or placebo, to 443 elderly males and females averaging 78 years of age. The study did not confine itself to heart failure patients, but due to the elderly demographic it was an outcome of interest.
As you might expect among an aged population, the prevalence of preexisting health conditions was high. Almost three-quarters had hypertension, 21% had diabetes, 23% had experienced previous thrombosis, 16% suffered a current or previous tumor, and 20% had NYHA class III heart failure.
The subjects were randomized to placebo or a combination of 200 mg/day of coenzyme Q10 capsules and 200 μg/day of selenium. The supplements were given for four years, with the first results reported after 5.2 years of follow-up.
As in the Q-Symbio trial, the CoQ10 supplement was Pharma Nord’s Bio-Quinone.
Selenium was administered as a patented selenium yeast product called SelenoPrecise.
The study was partly funded by Pharma Nord.
At 48 months, mean serum levels of CoQ10 levels in the supplemented group rose from 0.82 mg/l at baseline to 2.19 mg/l, while selenium levels rose from 66.5 to 210.3 mcg/l.
During 5.2 years of follow-up, 12.7% of treatment subjects and 16.2% of placebo participants died, a hazard ratio of 0.76. However, the difference was not statistically significant.
A statistically significant reduction of cardiovascular mortality was found in the treatment group versus placebo group (5.9% versus 12.6%).
N-terminal prohormone of brain natriuretic peptide (NT-proBNP) is a prohormone whose levels in the blood are used for screening and diagnosis of heart failure. At 48 months, NT-proBNP levels were significantly lower in the treatment group compared with the placebo group (mean 214 ng/L versus 302 ng/L, respectively).
Participants also underwent echocardiography, with a significantly better cardiac function score found in the supplementation group compared to the placebo group.
It was a win for the CoQ10 + selenium group, but the study was small and statistically underpowered. Of the 443 subjects who began the study, only 224 had data for analysis by the end of the follow-up period. Ninety-seven participants withdrew in the treatment group, and 118 in the placebo group.
In 2018, the researchers released a 12-year follow-up report. A significantly reduced cardiovascular mortality could be seen in those who were supplemented with CoQ10 and selenium; 28.1% in the treatment group versus 38.7% in the placebo group (HR: 0.59).
As for overall mortality, data from the National Board of Health and Welfare in Sweden showed 121 of the original 221 treatment subjects had died, compared to 141 of the 222 placebo subjects (54.7% versus 63.5%, respectively).
CoQ10 and Cancer
I have not been able to find any randomized clinical trials examining mortality outcomes in which CoQ10 or placebo was given to individuals with, or at high risk of, cancer.
A number of observational studies have been published in which subjects given CoQ10 were reported to have enjoyed higher-than-expected survival times. These reports lack blinding and control groups, and hence need replication in RCTs. Otherwise, we have no way of knowing with certainty that the results weren’t due to confounding from factors aside from supplementation.
A 1994 paper, of which the head author was employed by Pharma Nord, reported on 32 patients with breast cancer, aged 32-81 years and classified 'high risk' because of tumor spread to armpit lymph nodes. In addition to standard surgical and therapeutic treatment of breast cancer, the women were administered a combination of nutritional antioxidants (Vitamin C 2,850 mg, Vitamin E 2500 iu, beta-carotene 32.5 iu, selenium 387 mcg plus secondary vitamins and minerals), essential fatty acids (1.2 g gamma linolenic acid and 3.5 g n-3 fatty acids) and CoQ10 (90 mg per day).
Compliance was described as “excellent.” The authors reported that during eighteen months of follow-up:
None of the patients died during the study period (the expected number was four);
None of the patients showed signs of further distant metastases;
Quality of life was improved (no weight loss, reduced use of pain killers);
Six patients showed apparent partial remission.
In one of the six cases of remission, the CoQ10 dosage was increased to 390 mg. In one month, the tumor was no longer palpable and in another month, mammography confirmed the absence of tumor. Another patient, after non-radical surgery and with verified residual tumor, was then treated with 300 mg of CoQ10. After three months, the patient was in "excellent clinical condition and there was no residual tumor tissue."
A 2009 paper reported on forty-one end stage cancer patients in the setting of a Danish private practice. The patients were given, in addition to their standard treatment, a supplementation regimen consisting of:
CoQ10 300 mg
Selenium (as selenomethionine) 487 mcg
Folic acid 5 mg
Vitamin A 25,000 IU
β-carotene 76 mg (127,000 IU)
Small amounts of vitamins C and E, B complex vitamins, fish oil and gamma-linoleic acid were also administered (GLA was an overhyped fatty acid supplement that was popular during the late 80s and early 90s).
The type of CoQ10 formulation is not mentioned, but the paper’s “acknowledgement” section thanks Pharma Nord for supplying all medications free of charge. This would indicate the CoQ10 formula used was Bio-Quinone.
The antioxidant tablets were taken daily in two divided doses.
For safety reasons, patients with lung cancer did not receive β-carotene (a number of studies suggest increased lung cancer risk from taking large amounts of beta-carotene supplements).
Forty patients had died by the time the report was published; the fate of the remaining patient was unknown but was presumed to have died. The authors reported mean actual survival for the patients was 28.8 months, compared to a mean predicted survival of 11.9 months. Ten patients (24%) survived for less time than predicted, whereas 31 (76%) survived for longer.
It’s difficult to know what to make of these findings given it was an unblinded study with no control group. Predicted survival times were estimated mainly using data from the National Danish Cancer Registry. The authors note the Registry figures for breast cancer, inoperable renal cancer and advanced glioblastoma multiforme were inadequate and so other methods for estimating predicted survival times had to be employed. The accuracy of these estimates relies on the assumption that this group of 41 patients from a single practice was typical of Danish cancer patients in general. There’s no way of knowing if that is in fact the case. As a result, we don't whether some or all of the difference in predicted versus actual survival was due to the method of estimation and/or characteristics of the patient sample.
Numerous clinical trials have examined the effect of CoQ10 on various serum markers in diabetics, cancer patients, kidney and liver patients, with generally positive results and minimal to no side effects reported. However most were short-term studies and did not/were not able to report on mortality outcomes.
CoQ10 versus the Vaxxxines
The ‘COVID’ gene therapies have established a solid track record for causing cardiovascular damage (most notably, myocarditis and pericarditis) and sudden death. Given its promising results in heart failure, CoQ10 would seem a far more logical choice for vaxxx recipients than the ingredients currently included in hare-brained “Spike Support” formulas, which contain an array of doubtful and sometimes harmful substances (green tea extract, included in the Peter McCullough/Wellness Company formula, is notorious for causing liver toxicity).
In mice, pre-treatment with CoQ10 reduces both the severity of damage and mortality from experimentally-induced myocarditis. Whether CoQ10 counters the effects of globalist-induced myocarditis in humans remains to be seen.
In 2022, Italian researchers published a paper in which 174 “chronic COVID syndrome” patients were administered 100 mg of CoQ10 and 100 mg alpha lipoic daily (ALA) for 2 months.
The CoQ10 supplement was an Italian product called ReQupero which contains the ubiquinone form of CoQ10.
Average duration of the patient’s supposed “chronic COVID” was 5.9 months. Recruitment of patients took place between June 2021 to October 2021, well after the vaxxxine rollout kicked off in Italy. Given that symptoms of “long COVID” (in this case, fatigue, post-exertional malaise, disturbed sleep, impairment in cognition and balance) are often identical to those experienced by the vaxxx-injured, you would expect the authors to note how many of the participants were vaxxxinated, and whether their symptoms began or worsened after receiving the gene therapies.
Incredibly, the authors make no mention of vaxxxines and no information on vaxxxine status is included in the baseline data of the participants. Given the Pfizer vaxxx was rolled out on 27 December 2020 in that country, and by early June over 38 million doses of the gene therapies had been administered in Italy, there is simply no excuse for this.
The primary end-point was reduced fatigue, expressed as a reduction of at least 50% from baseline (which the authors deemed a ‘total response’) or at least 20% (partial response) in the Fatigue Severity Scale (FSS). Subjects showing less than 20% change were deemed non-responders.
Secondary end-points were changes in Visual Analogue Scale scores for pain, fatigue, sleep, the Widespread Pain Index, Symptoms Severity Scale and modified Fibromyalgia Assessment Status. Response for these scales was assessed in the same way as FSS response (responders, partial responders, non-responders).
After 2 months, a far higher number of those receiving CoQ10 + ALA were deemed responders on every scale. For the primary FSS endpoint, 53.5% of the supplemented group scored as responders, compared to only 3.5% of the control group.
The results sound impressive, but this was an unblinded study with no placebo, so we don’t know whether the results were swayed by placebo effect or researcher bias.
More Research Needed, But Don’t Hold Your Breath
The bottom line is that CoQ10 supplementation seems to reduce mortality in heart failure patients, although the evidence is of “moderate quality” as a recent Cochrane review described it.
The potential of CoQ10 to reduce cancer mortality has not been studied in randomized clinical trials. Ditto for mortality among kidney failure patients, another demographic that would seem a logical choice for CoQ10 supplementation.
As someone who you could fairly describe as a CoQ10 ‘believer,’ I find the lack of RCT research and data for CoQ10 frustrating. This is a nutrient that, based on what we know about its function and its inverse relationship with age and disease, would be expected to prevent or positively impact numerous diseases. It’s a supplement that we would reasonably expect to save lives, and lots of them.
CoQ10 is a supplement crying out for large-scale, long-term RCT scrutiny. Pharmaceutical companies have no incentive to study a non-patentable substance like CoQ10. At best, they won’t profit from it; at worst, it may endanger their profits by proving far more effective and far less harmful than the toxic drugs they peddle.
Supplement companies are not required to submit RCT data before bringing their products to market. Therefore, they have little to gain by conducting large-scale RCTs.
Governments, meanwhile, have well and truly established they are corrupt, thieving, treacherous entities penetrated by foreign forces who would much rather force you to receive toxic gene therapies than save your life. Combined with Big Pharma’s iron grip on the medical profession, this is a major reason why potentially life-saving strategies such as iron reduction and CoQ10 still remain woefully under-studied despite having being identified decades ago.
Summary
While most of the heart failure trials showing mortality reductions featured very small sample sizes, the results have consistently favoured CoQ10. The three moderately-sized trials (Morisco et al, Q-Symbio, KISEL-10) all showed reductions in both cardiac and overall mortality.
While I’d love to see confirmation of these findings in larger RCTs, I still consider CoQ10 a “non-negotiable” supplement for adults due to its critical role in cellular energy respiration and the decline in bodily levels seen with ageing.
In the next article, we’ll look at some of the marketing claims made for the various CoQ10 formulations and see if any really do offer superior absorption.
Leave a Reply